High-fat diets are LITERALLY depressing—here’s why
02/25/2020 / By Evangelyn Rodriguez

The World Health Organization (WHO) defines overweight or obesity as the abnormal or excessive accumulation of fat that presents a health risk. Obesity is caused by either one of two things: genetics or an increased consumption of high-calorie foods coupled with a sedentary lifestyle. People with obesity suffer from abnormalities characteristic of metabolic syndrome and an increased risk of chronic and fatal diseases like cancer. Studies have also linked obesity to depression, and the results of several clinical studies demonstrate a positive association between the two. However, the mechanism underlying this association is still unknown.
In a recent study published in the journal Translational Psychiatry, researchers from the U.S. and the U.K. investigated whether obesity is a causative factor for the development of depression. They also looked at possible molecular pathways that link the two disorders. The researchers found that genetically induced or diet-induced obesity leads to depression when a signaling pathway called the cAMP/PKA signaling pathway is disrupted, and this disruption results from the influx of saturated fatty acids in the brain, specifically in the hypothalamus. This influx is caused by the consumption of a fat-dense diet. The researchers also discovered that the loss of PDE4A, an enzyme that influences the development of obesity, can prevent both genetically induced and diet-induced depression-like behavior in mice.
The link between obesity and depression
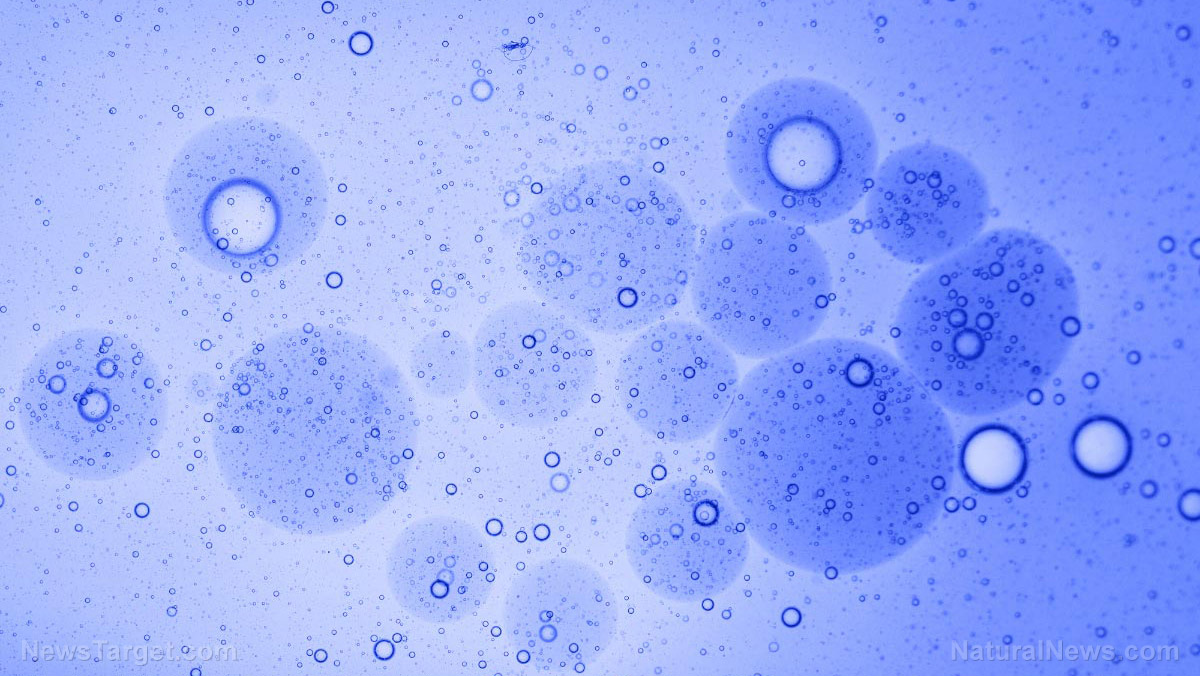
The 3′,5′-cyclic AMP (cAMP)/protein kinase A (PKA) signaling pathway is an important signal transduction pathway. cAMP is a secondary messenger molecule used by cells in response to stimulation from different hormones and neurotransmitters. cAMP plays a role in various cell functions, regulating important cell processes such as cell growth, differentiation, protein expression and gene transcription.
PKA, on the other hand, is an enzyme responsible for all the cellular responses facilitated by cAMP. It is often called an end effector of a variety of hormones that work via the cAMP signaling pathway. PKA activity is regulated by the concentration of cAMP in cells and involves the regulation of vital cell functions, such as the metabolism of glycogen, sugar and lipids. PKA also regulates different neuronal functions.
According to studies, cAMP signaling is impaired in depression by enzymes called phosphodiesterases (PDEs). These enzymes are responsible for degrading cAMP in cells. Among the many PDEs that exist, members of the PDE4 family, particularly PDE4A, play a major role in regulating cognition and depressive disorders. These enzymes also interact with a group of free fatty acid receptors (FFARs) in the brain that bind to dietary fatty acids of varying lengths and saturation. Dietary fatty acids regulate the melanocortin signaling pathway, the most important neuronal pathway for human obesity.
Using lipidomic and transcriptomic methods, the researchers successfully identified the mechanism that links the consumption of a high-fat diet (HFD) to alterations in hypothalamic function that lead to depression. They found that HFD selectively induces the accumulation of palmitic acid, the most common saturated fatty acid found in living organisms, in the hypothalamus. HFD not only suppressed the cAMP/PKA signaling pathway in mice, it also increased the concentration of FFAR1. Mice with impaired cAMP/PKA signaling due to the influx of fatty acids in their hypothalamus developed depression-like behavior.
On the other hand, the researchers found that a deficiency of PDE4A protected mice fed an HFD from genetic- or dietary-induced depression. (Related: Obesity causes depression, concludes “strongest evidence yet”.)
Based on these findings, the researchers concluded that consumption of saturated fats disrupts hypothalamic functions by suppressing cAMP/PKA signaling via the activation of PDE4A. With this mechanism in mind, they believe that inhibiting FFAR1 and/or increasing cAMP signaling is a potential therapeutic target that can counteract the effects of genetically induced or diet-induced obesity on depression.
Sources include:
Tagged Under: brain function, brain health, depression, genetics, high-fat diet, hypothalamus, mental health, obesity, poor nutrition, research
RECENT NEWS & ARTICLES
COPYRIGHT © 2017 RESEARCH NEWS