Study: 55% of coronavirus cases in long-term care facilities in Maryland were ASYMPTOMATIC at the time of testing
07/27/2020 / By Arsenio Toledo

More than half of nursing home residents in Maryland that have tested positive for the Wuhan coronavirus (COVID-19) did not have any symptoms at the time of testing.
According to a report by the The New York Times, more than 40 percent of coronavirus-related fatalities in the United States have come from long-term care facilities, such as nursing homes, memory care facilities, assisted-living facilities, rehabilitation centers and retirement and senior communities.
Because these facilities have emerged as coronavirus hotspots, a team of researchers from Johns Hopkins University (JHU) set out to determine how the deadly virus was able to spread largely undetected through these institutions.
“My thought in doing this is that we had an opportunity in the nursing home setting to be South Korea – to provide widespread testing, really identify the burden of disease and then try to isolate based on that,” said Morgan Katz, one of the authors of the study and an assistant professor of medicine at JHU’s School of Medicine.
Katz and her colleagues decided to study nine nursing homes and two assisted-living facilities in Maryland that had confirmed COVID-19 cases.
Initially, these facilities had 153 cases that were identified through targeted, symptom-based testing. When the researchers tested the remaining 893 residents, they found an additional 354 cases of COVID-19, which meant that more than half of the residents in these 11 long-term care facilities had the coronavirus.
According to the study, around 55 percent of all the infected residents were asymptomatic at the time of testing. Many of these positive residents developed serious illnesses soon afterward.
Katz’s team followed up on seven of the facilities after two weeks and found that 20 of the 154 then-asymptomatic patients required hospitalization, while seven passed away due to COVID-19 complications.
Katz believes their research highlights the necessity of following the guidelines set by the the Centers for Disease Control and Prevention (CDC), which require all residents and staff members of nursing homes to be tested if even one positive case is found. Unfortunately, the federal government only requires facilities to report infections and deaths and does nothing but offer recommendations on how often they should conduct COVID-19 tests on their residents.
Many states have different policies on testing nursing home workers, and some states like California are beginning to reopen even their nursing homes to allow visitors to come and go. Katz believes that this policy reduces the efficacy of one-time baseline testing, and what these facilities need are “on-site tests with rapid turnaround times so they really can respond immediately to any potential outbreaks.” (Related: Cuomo claims nursing home outbreaks spread by workers, not his directive that FORCED facilities to bring in more coronavirus patients.)
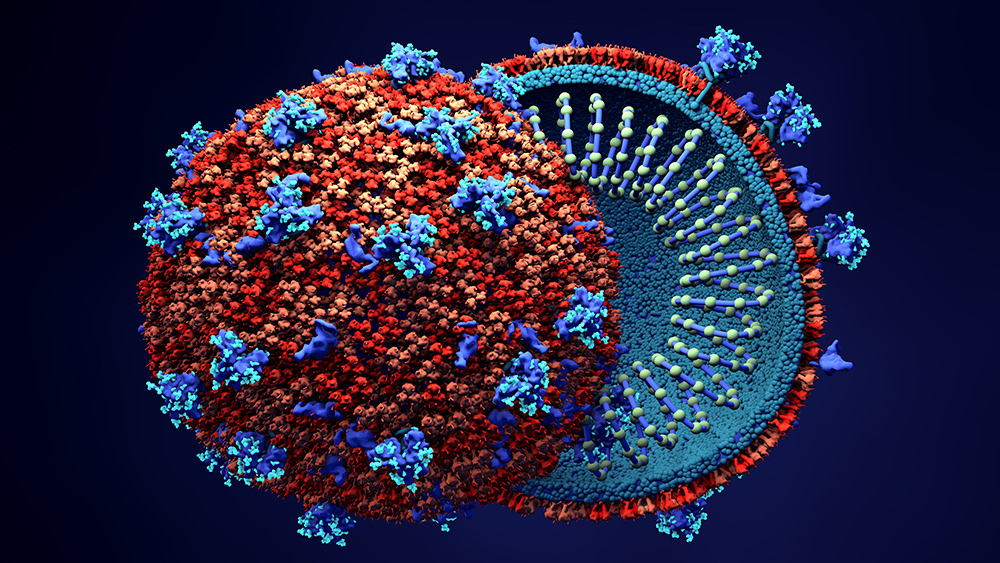
Watch this episode of Brighteon Conversations with Mike Adams, the Health Ranger, as he has a very engaging and illuminating discussion with Dr. Paul Cottrell about a new strain of the Wuhan coronavirus known as “D614G,” which spreads a lot more easily than older variants of COVID-19.
One Maryland nursing home able to repel the coronavirus by acting quickly and locking down the facility
While many long-term care institutions in Maryland have to deal with rising COVID-19 cases within their facilities, the Maryland Baptist Aged Home in Baltimore has not reported a single case of infection since the beginning of the outbreak in America.
The head of the facility, Rev. Derrick DeWitt, said that the key to his nursing home’s success was early mitigation, and the application of proactive protocols that prevented the coronavirus from entering. Back in February when the U.S. only had around 15 cases, the nursing home sprung into action before the rest of the country even began locking down.
On March 1, the nursing home went into a full lockdown. Visitors were not allowed to enter the facility, and they instituted a very thorough, rigorous screening process for their employees, which included providing the facility with the details of where the workers were during their time off, the regular taking of body temperatures and the wearing of protective gear – masks, gowns and gloves – whenever they had to come into contact with any of the home’s residents.
Maryland Baptist also benefited from the fact that DeWitt hired a full-time quality assurance and infection control nurse who set up many of the anti-coronavirus measures the facility greatly benefited from.
Lastly, DeWitt cared for the emotional well-being of his residents by bringing in extra activity staff who made sure that the residents had visitors to interact with on a daily basis. He even hired a chef who came to help his staff prepare the residents’ meals and make them more pleasing.
The story of Maryland Baptist and Rev. DeWitt’s quick response to the pandemic shows how institutions can keep the coronavirus outside of their walls.
Maryland Baptist’s success is a bright spot in the otherwise bleak events that have affected nursing homes all across the country. According to The New York Times, at least 296,000 residents in long-term care facilities have contracted the coronavirus, and 55,000 have died.
If long-term care facilities learn from Maryland Baptist’s example and apply Katz’s recommendation to conduct regular and rapid COVID-19 testing on nursing home employees and residents, future fatalities in many nursing homes could be prevented.
Learn about how other institutions are fighting back against the coronavirus by reading the articles at Pandemic.news.
Sources include:
Tagged Under: America, anti-coronavirus measures, asymptomatic infections, coronavirus, covid-19, government, infection control, infections, infectious diseases, lockdown, long-term care facilities, maryland, mass testing, nursing homes, outbreak, pandemic, research, testing
RECENT NEWS & ARTICLES
COPYRIGHT © 2017 RESEARCH NEWS