The SHOCKING truth about antacids and their effect on your gut health
06/18/2020 / By Divina Ramirez

Acid-reducing agents (ARAs) like antacids and proton pump inhibitors (PPIs) are some of the most common medications prescribed for the treatment of heartburn. A recent study published in the Journal of Clinical Biochemistry and Nutrition found that long-term use of PPIs leads to a decrease in the amount of Faecalibacterium, one of the most beneficial bacteria in the human gut.
Long-term use of PPIs also leads to the proliferation of Streptococcus, a genus of bacteria linked to numerous infections including strep throat and pneumonia.
Gastric acid and heartburn
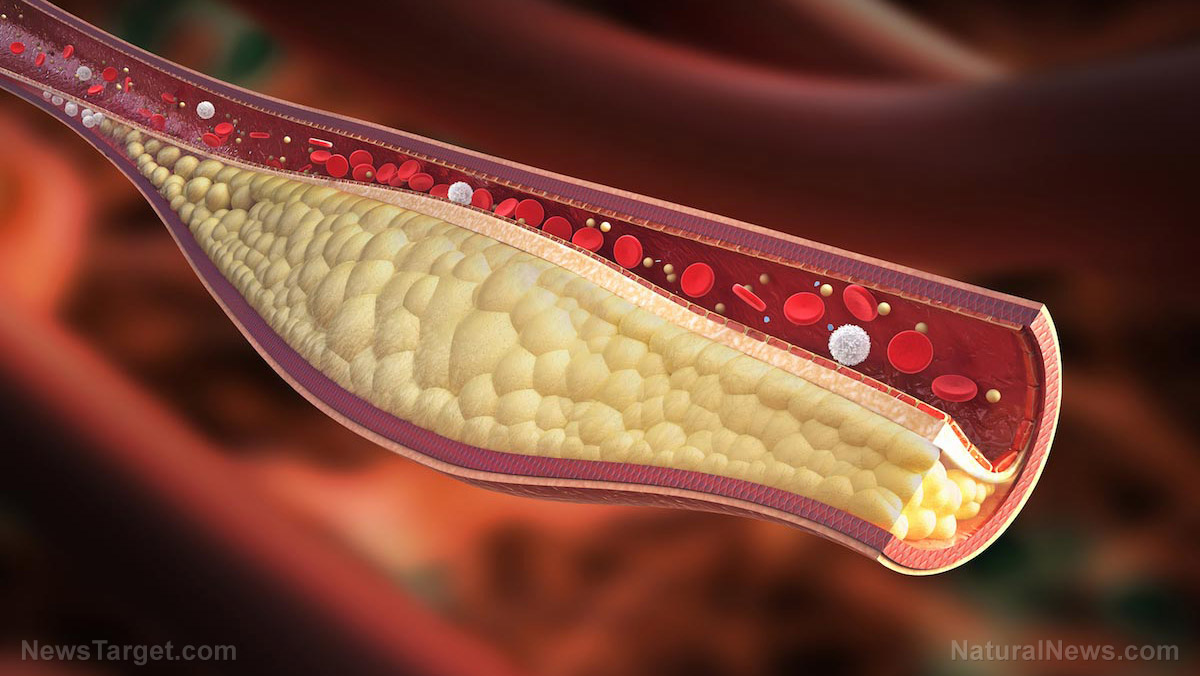
Gastric acid plays an important role in digestion. It breaks down food and improves the absorption of proteins, vitamins and other essential nutrients. Gastric acid also helps neutralize harmful bacteria and other pathogens in the stomach to prevent infection.
In some cases, the contraction of muscles around the esophagus can cause gastric acid to back up into the esophagus from the stomach, causing a burning sensation to spread across the chest. This is called heartburn or acid reflux.
Certain foods and drinks can trigger this action, including spicy foods, acidic foods, fried foods, alcohol, coffee and carbonated drinks.
For the most part, heartburn is no cause for concern. It might take a few hours to subside depending on the cause, but it does disappear on its own.
That said, frequent heartburn may be a sign of gastroesophageal reflux disease (GERD), a digestive condition common in pregnant women and overweight individuals. Because frequent heartburn can be a painful inconvenience, many people who suffer from GERD tend to use antacids to treat heartburn fast.
If the heartburn is quite severe, a physician may prescribe PPIs. These medications work much like antacids but with stronger acid-reducing effects, neutralizing stomach acids and eliminating trapped gas in the stomach. (Related: Antacid drugs linked to increased risk for heart attack, dementia and renal failure.)
The adverse effects of PPIs on gut health
Researchers from the Kyoto Prefectural University of Medicine and Takara Bio Inc. in Japan found evidence that long-term use of PPIs has harmful effects on gut health and microbiota.
To understand the mechanisms behind these effects, the researchers studied 36 patients from the Kyoto Prefectural University of Medicine‘s outpatient clinic who used PPIs for at least a year prior to the study. They also studied 36 non-users of PPIs as control subjects.
They then collected fecal samples from all of the participants and checked these for the presence of bacteria. After analyzing the samples, the researchers found that PPI users had a lower amount of Faecalibacterium in the gut.
Faecalibacterium is one of the most abundant beneficial bacteria in the gut. This bacterium helps maintain intestinal health and guard against inflammation linked to gastrointestinal conditions, such as ulcerative colitis and Crohn’s disease. Therefore, low levels of this beneficial bacterium can make the gastrointestinal tract susceptible to inflammation and infection.
The researchers also discovered that the long-term use of PPIs encouraged the growth and spread of Streptococcus bacteria. Most of the species that belong to this genus are linked to infections like strep throat, which is marked by inflamed tonsils and enlarged lymph nodes in the neck. Streptococcus bacteria have also been linked to community-acquired pneumonia.
Based on their findings, the researchers concluded that the long-term use of PPIs affects the bacterial communities in the gut. It follows, then, that PPI use has negative effects on overall gut health.
Sources include:
Tagged Under: acid reflux, antacids, bad gut bacteria, bad medicine, digestion, digestive health, Faecalibacterium, good gut bacteria, gut microbiota, harmful medicine, heartburn, infections, inflammation, Prescription drugs, Proton pump inhibitors, research, Streptococcus, superbugs
RECENT NEWS & ARTICLES
COPYRIGHT © 2017 RESEARCH NEWS