Inflammation: The key link between the vicious cycle of depression and heart disease
07/30/2019 / By Evangelyn Rodriguez

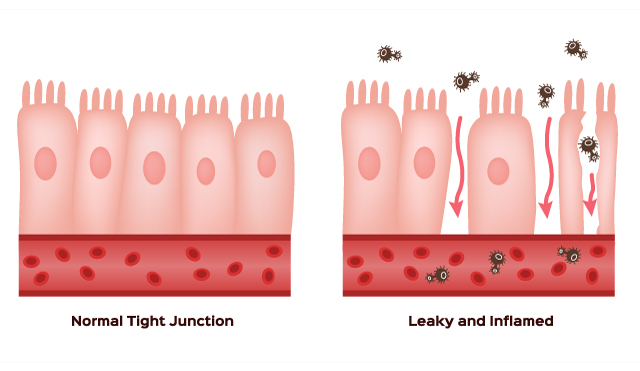
Inflammation is part of your body’s immune response. While this natural process helps protect the body from infection, it can also cause harm when it lasts for too long. Chronic inflammation is linked to the development of serious health conditions, such as heart disease, diabetes, obesity, and cancer. Inflammation also affects mental health and has been associated, by many studies, with major depressive disorder (depression). In a new study published in Molecular Psychiatry, researchers from the University of Cambridge in the U.K. reported a surprising discovery: They found a connection between heart disease and depression – and the link between these two conditions happens to be inflammation.
The link between depression, heart disease, and inflammation
Heart disease and depression often go hand-in-hand. According to numerous studies, people who suffer from heart disease often manifest symptoms of depression. Meanwhile, people with major depressive disorder also have a higher risk of developing heart disease. Despite the obvious connection between the two, scientists have struggled to identify the missing link responsible for their comorbidity. (Related: Depression May Cause Heart Disease and Related Death.)
For years, researchers have conjectured that heart disease and depression share common genetic or environmental factors. However, Golam Khandaker, one of the authors of the present study, believed that it is more likely that the two conditions share common underlying biological mechanisms, which “manifest as two different conditions in two different organs — the cardiovascular system and the brain.”
“Our work suggests that inflammation could be a shared mechanism for these conditions,” said Khandaker.
For their study, Khandaker and his team analyzed data from more than 300,000 participants of a long-term study known as the U.K. Biobank. They considered the participants’ family history of coronary heart disease and their risk of depression. They also calculated a genetic risk score for coronary heart disease for each individual and examined its association with depression risk.
The researchers found a connection between family history of heart disease and an individual’s risk of depression. Specifically, participants who reported losing at least one parent to heart disease had a 20 percent higher risk of developing depression symptoms at some point in their life. On the other hand, the researchers found no relationship between genetic predisposition for heart disease and the likelihood of having depression. This suggests that heart disease and depression are not linked by genetic factors but by environmental ones.
The researchers continued their investigation by using statistical analysis to examine biomarkers associated with coronary heart disease. Of the 15 they considered, they identified three biomarkers – triglycerides, interleukin-6 (IL-6), and c-reactive protein (CRP) – that also serve as risk factors for depression. Both IL-6 and CRP are known inflammatory markers. According to previous studies, patients with treatment-resistant depression or acute depressive episodes have high levels of IL-6 and CRP in their blood. High levels of these biomarkers can also increase a person’s risk of depression.
Dr. Stephen Burgess, a colleague of Khandaker and co-author of the study, said that while the shared mechanisms behind heart disease and depression remain unknown, their findings point to the involvement of the immune system.
“Identifying genetic variants that regulate modifiable risk factors helps to find what is actually driving disease risk,” said Burgess. Their team strongly believed that, due to these markers’ association with both conditions, triglycerides, IL-6, and CRP are attractive targets for the treatment and prevention of heart disease and depression.
The role played by triglycerides in coronary heart disease is already well-established; however, the role they play in major depressive disorder is yet to be explored. This is another subject that needs to be focused on by future studies.
As for the implications of the study findings, the experts believed that they provide enough evidence that physical and mental health are deeply related and should no longer be considered separately when it comes to research or treatment.
Sources include:
Tagged Under: breakthrough, comorbidity, cool science, coronary heart disease, depression, discovery, heart health, immune response, inflammation, inflammatory markers, major depressive disorder, Mental Disorders, mental health, mind body science, prevention, research
RECENT NEWS & ARTICLES
COPYRIGHT © 2017 RESEARCH NEWS