Alzheimer’s hits more than just the memory; patients experience immune system dysfunction as well
01/06/2019 / By Michelle Simmons

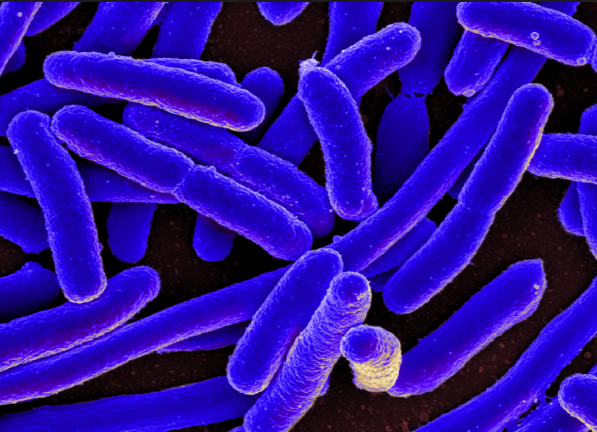
Researchers have discovered that there is a link between inflammation biomarkers in both plasma and cerebrospinal fluid and markers of Alzheimer’s disease-associated pathology. This means that the disease does not only affect memory, but the immune system of patients as well.
The study was conducted by a group of researchers from the University of Colorado Anschutz Medical Campus, together with the University of Wisconsin Alzheimer’s Disease Research Center and the University of California San Francisco Memory and Aging Center.
Past research has suggested that pathology related to Alzheimer’s disease may develop before its clinical symptoms become evident, and that inflammation is a primary component of the disease. Moreover, links between the levels of inflammatory markers in cerebrospinal fluid and blood and mild cognitive impairment were revealed in previous studies. Furthermore, researchers discovered that increases in inflammatory markers may occur even decades before any symptoms of Alzheimer’s disease manifest. (Related: Predicting Alzheimer’s: Major inflammation in your 40s puts you at high risk, making the case for improving lifestyle habits.)
The research team analyzed the relationship of inflammatory markers in cerebrospinal fluid and plasma to see how well plasma inflammatory markers indicate central nervous system inflammation. They also identified whether plasma inflammatory markers were separately associated with cerebrospinal fluid markers of Alzheimer’s-related pathology and neuronal damage. In the study, they investigated blood and cerebrospinal fluid samples of 173 middle-aged and older adults in the Wisconsin Alzheimer’s Disease Research Center. The participants were healthy and did not have clinical symptoms of Alzheimer’s disease, although several had family records of dementia presumed because of the disease.
The researchers expected inflammation markers in the cerebrospinal fluid to be more powerful predictors of Alzheimer’s disease-related pathology and neuronal damage in comparison to those in the blood because of the “blood brain barrier.” However, the study revealed that inflammation markers in blood plasma as well as those in cerebrospinal fluid independently pass on information about Alzheimer’s-related pathology and neuronal damage.
“From my perspective, there has been a perception in the field that the blood and the ‘periphery’ are not related to the brain – that the brain and the rest of the body are completely separate,” explained Brianne Bettcher, one of the study authors.
Bettcher believes their findings indicate that inflammation markers in the blood show signs of what is going on inside the brain. Moreover, the study points to a possible early role for inflammation in aging and Alzheimer’s, although the presence of inflammation markers alone does not suggest a diagnosis of the disease, nor does it indicate that Alzheimer’s will develop later on.
Preventing Alzheimer’s disease
In 2017, approximately 5.5 million people in the U.S. were found to suffer from Alzheimer’s disease. Moreover, the disease has been identified as the sixth leading cause of death in the country. The prevalence of Alzheimer’s is alarming, thus, it is essential to identify how to prevent its onset. Here are some ways to prevent Alzheimer’s disease.
- Exercising regularly – Exercise can reduce the risk of developing Alzheimer’s disease and can hamper further deterioration in those who have already started to develop cognitive problems.
- Engaging in social activities – Social engagement may protect against Alzheimer’s and dementia later in life.
- Following a healthy diet – Inflammation and insulin resistance damage neurons and hinder communication between cells. Eating healthy food can help reduce inflammation and support brain health.
- Exercising your brain – Engage in brain-challenging activities and try to learn new things to improve cognitive function and prevent cognitive decline.
- Having quality sleep – Disrupted sleep is both a symptom and a potential risk factor for Alzheimer’s. Thus, having a good quality sleep may prevent the disease.
- Relieving stress – Being stressed out for a long time can damage the brain, resulting in shrinkage in a key memory area, preventing nerve cell growth, and increasing the risk of Alzheimer’s disease and dementia.
Read more studies on Alzheimer’s disease at Alzheimers.news.
Sources include:
Tagged Under: Alzheimer's disease, brain function, brain-body communication, immune system, inflammation, mental health, mind body science, neurology, research