Antibiotic resistance isn’t just a “human” problem: Study shows it can be passed along to pets
09/10/2019 / By Lance D Johnson

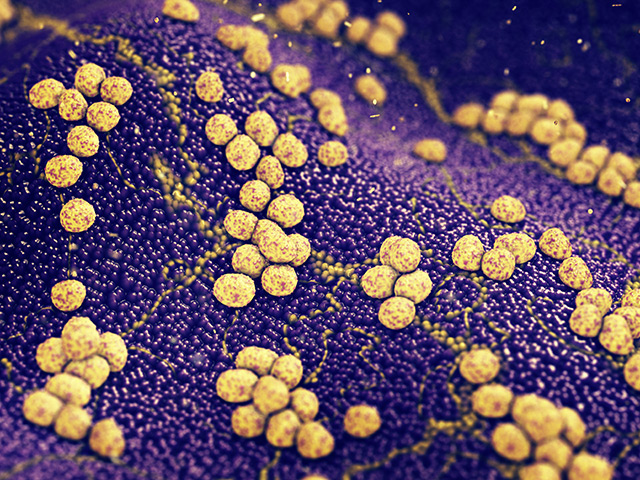
The genetic evolution of bacteria is occurring at a rapid pace, and aberrations of bacterial DNA are transferring from one species to the next. These genetic deviations, spurred by antibiotics, are now transferring from humans to animals. For the first time ever, researchers have isolated antibiotic-resistant bacteria samples from household pets. Recently, a U.K. animal hospital obtained highly evolved bacteria samples from cats and a dog. The bacterium has a new gene that allows it to resist linezolid, an antibiotic that is used to treat streptococci and methicillin-resistant staphylococci (MRSA) in humans. This antibiotic is not even used on animals in the U.K., but the resistant gene is showing up now in U.K. pets. This is the first sign that the gene (optrA) can spread between the microbiome of humans and animals and vice versa.
“We believe this is the first report of optrA-positive enterococci isolated from companion animals in the U.K.”, says lead researcher Dr Katie Hopkins from Public Health England. “This is concerning as transmission of this organism to owners carries the potential for spread to other bacteria, including Staphylococcus aureus. This may lead to difficult-to-treat infections.” Dr. Hopkins says that all veterinary surgeons must be aware of this and ensure adequate disinfection takes place. Dr. Hopkins also believes that humans should wash their hands after handling their pets.
Resistant genes can be swapped between bacteria species using DNA plasmids
It’s likely that the bacteria that resist linezolid gained their new survival traits in the pets from similar optrA gene resistance associated with florfenicol, an antibiotic that is used in animals. For the most part, these resistant genes are contained within chromosomes, making it nearly impossible to spread from one species of bacteria to the next. However, recent discoveries have found that these resistant genes are replicating in plasmids, which are mobile DNA pieces that can travel between bacteria populations. The mutation known as optraA has been identified on plasmids. Medical professionals are worried about widespread mutations like this because it could mean there is an apocalypse on the horizon, wiping out any remaining effectiveness for current antibiotic treatment protocols.
Dr Hopkins warns that, even though linezolid resistance is rare, “Transmission of this organism to owners carries the potential for plasmid-mediated spread to other bacteria, particularly in healthcare environments.”
The mutations were discovered during routine testing of a cat wound at a U.K. animal hospital. The sample of Enterococcus faecalis was sent to Public Health England’s Antimicrobial Resistance and Healthcare Associated Infections Reference Unit along with three similar bacteria samples obtained from two other cats and one dog from different households. The bacteria were resistant to linezolid and gentamicin, an antibiotic used to treat eye infections and infections of the heart and central nervous system. The researchers were able to stop its infectivity using antibiotics teicoplanin, vancomycin, and daptomycin, but one must wonder how long will it takes the bacteria to evolve to resist all these antibiotics? (Related: Emerging superbug kills woman: Infection resistant to 26 antibiotics.)
Dr. Hopkins said the findings further prove “that antibiotic-resistant bacteria can be shared by animals and humans” even though the “direction of transfer is often difficult to prove.” The researchers do not know how common these resistant enterococci are in pets and therefore call on a joint approach for “emergence and dissemination of resistance mechanisms of public health importance.”
For more on this topic, check out Superbugs.News.
Sources include:
Tagged Under: animal health, antibiotic failures, antibiotic resistance, Antibiotics, bacteria evolution, discoveries, DNA plasmids, linezolid resistance, microbiome, mutation, outbreak, pandemic, pet health, Public Health, superbugs
RECENT NEWS & ARTICLES
COPYRIGHT © 2017 RESEARCH NEWS